Hypoplastic Left Heart Syndrome (HLHS)
Hypoplastic left heart syndrome (HLHS) is a serious problem that involves several parts of the left side of the heart. It is quite rare and occurs in about 1 out of every five thousand babies born. In the United States, about 1000 babies with HLHS are born each year. Two thirds of the babies affected are boys. Most babies with HLHS are otherwise healthy but some have other medical problems including other heart problems, neurologic problems, and Turner's syndrome.
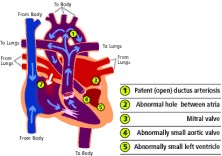
In this condition, for unknown reasons, the left side of the heart does not develop properly while the baby is in the mother's womb. The parts of the heart that are usually affected are the mitral valve (1), the left ventricle (2), the aortic valve (3), and the aorta (4) In the normal heart, red blood returning from the lungs, flows from the heart's left upper chamber called the left atrium through the mitral valve to the left ventricle where it is pumped through the aortic valve and out to the body. In babies with HLHS, the left side of the heart is underdeveloped and cannot pump enough blood to meet the body's needs.
Without treatment, 95% of babies with HLHS die within the first month of life. Treatment means either three heart surgeries during the first two years of life or a heart transplant. Due to dramatic improvements in surgery and medical care, many children born with HLHS now do very well. However, these treatments involve many stressful experiences and risks. The treatments are not a "cure" and the children will need expert medical attention for the rest of their lives.
What are the effects of this defect on my child's health?
Like most heart defects, HLHS does not have an adverse affect until after the baby is born. Prior to birth, the baby's oxygen comes from the mother and the baby's lungs are filled with fluid. Blood pumped from the baby's right side of the heart bypasses the lungs by flowing through a blood vessel called a patent ductus arteriosus. Usually, one to two days after birth, this vessel closes. In a baby with HLHS, closure of the ductus arteriosus removes the baby's means of supplying blood to the body and results in shock and death. If the diagnosis of HLHS is made, a medicine given through the vein called prostaglandin is used to keep the ductus arteriosus from closing until the time of surgery. See the sections on heart transplantation and three stage surgical repair for information on health outcomes after treatment.
Participation in physical activities and sports: Children who undergo surgical repair of HLHS can participate in recreational physical activities but are restricted from competitive and vigorous athletic activities.
How is this defect diagnosed?
Prenatal diagnosis: The diagnosis of HLHS is made by an echocardiogram or ultrasound of the baby's heart and can be made as early as 16 weeks into the pregnancy. An echocardiogram of the heart is done when a possible problem is identified during a routine prenatal ultrasound or because of a family history of congenital heart disease. Left sided heart problems tend to recur in families where one child is affected. Estimates of having another child affected range from 4.5 to 13% (Boughman et al. 1993, Brenner et al. 1989). If there is a family history or if concern is raised during a routine ultrasound, the family is referred to a pediatric cardiology center where a detailed ultrasound of the heart is performed.
Clinical features: Most newborns with HLHS have mild heart related symptoms until the patent ductus arteriosus closes. This usually occurs within 48 hours of birth. Prior to closure of the ductus arteriosus, the baby's lips or fingernails may look slightly blue, especially when the baby cries. Babies with HLHS often breathe fast, have low energy levels, and/or have feeding problems. These changes can be subtle and can be difficult to detect in a newborn baby. When the ductus arteriosus does close, the baby may get very ill very quickly and develop symptoms of shock
Physical findings: The presence of a heart murmur, mild cyanosis (blue color from low oxygen levels in the blood), fast heart rate, and fast breathing rate are the first clues that an infant has HLHS.
Medical tests: The first tests often ordered are an electrocardiogram, chest x-ray and oxygen saturation test. The electrocardiogram may show decreased left-sided forces. The oxygen level in the blood is usually a little low. The chest x-ray often shows a bigger than normal heart and extra blood flow to the lungs. The gold standard for diagnosis is an echocardiogram. Cardiac catheterization is done if there are any questions not clearly answered by the echocardiogram.
How is hypoplastic left heart treated?
Treatment of HLHS means either a three-staged surgical repair or heart transplantation.
Three-stage surgical repair for HLHS
The surgical repair for HLHS is a series of three heart operations done during the first two years of life. The goal of these operations is to rebuild the heart so that the right side can be used to pump blood out to the body. The first operation is done during the first week of life, the second one is done when the child is four to six months old, and the last one is done when the child is about two years old.
In addition to the three operations, two or three heart catheterizations must be done. A heart catheterization is a heart test that is done by a cardiologist with the help of cardiovascular technicians. Soft, thin plastic catheters (tubes) are placed in the large blood vessels in the leg and threaded carefully to the heart. The catheters are used to take pressure measurements inside the heart and to inject contrast or dye so pictures of the heart can be taken. Overall, this is a very safe test and children can go home the same day.
Heart Transplantation for Hypoplastic Left Heart Syndrome
Heart transplantation is one option for treatment of children with hypoplastic left heart syndrome and remains an option even after staged surgical repair. Heart transplantation means that the heart from a child who died is removed and used to replace the defective heart in someone with a very serious heart problem. The first heart transplant was done in an adult in 1967. While early results were encouraging, most people died within one or two years after transplantation because the immune system rejected the new heart. In the early 1980’s, a new anti-rejection drug called cyclosporine became available and proved to be very effective in preventing rejection of transplanted hearts as well as other transplanted organs. In 1985, Dr. Leonard Bailey at Loma Linda University demonstrated that heart transplantation could be successfully done in infants with HLHS and other serious heart problems.
Heart transplantation offers advantages and disadvantages in the treatment of children with HLHS. Unlike children who undergo the three stage reconstructive approach, children who undergo transplant need one operation during early childhood that results in a "normal heart", that is, a heart with four chambers that pumps in the normal way. The risks associated with the operation itself are quite low at most major centers. Operative risk with the three stage surgeries varies considerably across institutions and in some centers it is very high.
Disadvantages of heart transplantation include the lack of availability of donated hearts of a size suitable for an infant. Due to the numbers of children awaiting heart transplantation and the lack of availability, about 10-25% of children die awaiting transplantation. Other concerns include side effects from the life long need for anti-rejection medications, growth problems, and early onset coronary artery disease. Also, low-grade rejection is almost inevitable so that the average "lifespan" of a transplanted heart is about ten years. For more information on heart transplantation, click here.
What is the prognosis for children with hypoplastic left heart syndrome?
The outlook for children with HLHS has improved dramatically. While once uniformly fatal (with 95% mortality by one month of age) survival at 3 to 5 years of age is now about 60%. Most children enjoy a good quality of life without significant developmental problems Although the outlook has improved, decision-making about treatment is difficult due to the potential for suffering and distress associated with multiple surgeries and heart catheterizations and high medical costs, particularly in light of an uncertain long term outlook for the children. Our experience so far indicates that most children will reach adulthood in good health. Some children will need other surgical procedures such as a pacemaker for abnormal heart rhythms. Some children will need a heart transplant at some point in the future. Children are restricted from competitive sports and from very demanding physical activities but can otherwise do all the things that children enjoy doing. Overall, it is expected that these children have a good quality of life: have friends, play, and go to school just like other children.
Stage 1: The Norwood Operation
The Norwood is the first of the three heart operations. It is most often done during the first week of life.
Why is the Norwood operation done?
Since the heart's left side does not pump well, the heart is rebuilt so the right side of the heart becomes the main pumping chamber. After the Norwood, the right ventricle pumps blood to both the lungs and the body.
How is the Norwood operation done?
The blood vessel leaving the right side of the heart called the pulmonary artery is divided. The far end (the end closest to the lungs) is sewn shut. The near end (the end closest to the heart is sewn into the aorta, which is the large blood vessel leaving the left side of the heart. A patch is sewn in this area to make the "new aorta" or neo-aorta bigger and stronger. Now all the blood leaving the heart goes from the right side of the heart through the pulmonary valve and out to the body through the new aorta (1).
A hollow tube that connects the new aorta to the pulmonary artery is sewn in place (2). The tube is called a Blalock-Taussig (BT) shunt. The BT shunt lets some of the blood pumped to the body go to the lungs.
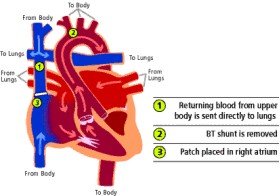
The wall between the heart's two upper chambers is removed (3). This allows red blood coming back from the lungs to flow from the left upper chamber to the right upper chamber. The blood then goes to the right lower chamber and out to the body.
After the Norwood operation
After the Norwood operation, the right heart pumps a mixture of red and blue blood out to the body. It pumps blue blood coming back from the body and red blood coming back from the lungs. Since mixed blood is going out to the body, the oxygen level in the blood is lower than normal. This makes the baby's lips look a little "dusky" or blue and is more noticeable when the baby cries. Since the baby's body is used to a lower oxygen level, it does not hurt him to cry even he looks bluer.
Most babies go home ten days to two weeks after the Norwood operation is done. They often go home on three or four heart medicines. Some babies need to use a feeding tube for part of their feedings, at least for the first several weeks. Babies with heart problems often need extra calories in their milk. Breast milk is very good for children with heart problems as it is for all babies. Mothers of babies with heart defects can breast feed and breast milk can be given in the tube feedings. Supplements can be added to the breast milk if the baby needs more calories.
Parents learn about their baby's care before discharge from the hospital. They will be able to feed their baby and give the medicines that will be needed at home. In this way, parents come to know that they can care for their baby's special needs. Many parents choose to have a nurse visit their home after the baby leaves the hospital. The nurse can answer questions, assess how the baby is doing, and help parents learn more about their baby's care.
After the Norwood, most babies grow well and learn to smile, roll over, and play with their toys like other babies. Some babies have trouble gaining weight and need richer milk to drink. Some are slow to learn motor skills. Babies who are slow to develop often benefit from special help that can be arranged through the local school district, among other places.

1 Comments:
I was surfing around (or whatever it is you call it when you are looking thru blogs). I thought I'd encourage you. My daughter has been through the Norwood, the Glenn, and even the Fontan. We are 4 yrs down the road from where you are (thankfully w/o the Gloria type fiascos). Life can get good again. The first year is the hardest one. Then things get oddly normal. You probably have come across some great resources already, but just in case, I want to suggest Deb Hilton's www.hlhsinfo.org . I'll keep your family in our prayers.
Post a Comment
<< Home